By Prof. Avindra Nath and Dr Bridgette Jeanne Billioux, Tropical and Geographical Neurology Specialty Group
Over the past month we have reviewed the pertinent literature and news, and present this month's Neurology and Covid update. Several topics were at the forefront of Neurology and Covid news, including longitudinal neurologic imaging of COVID-19 patients' brains and long-term cognitive evaluations in COVID-19 survivors.
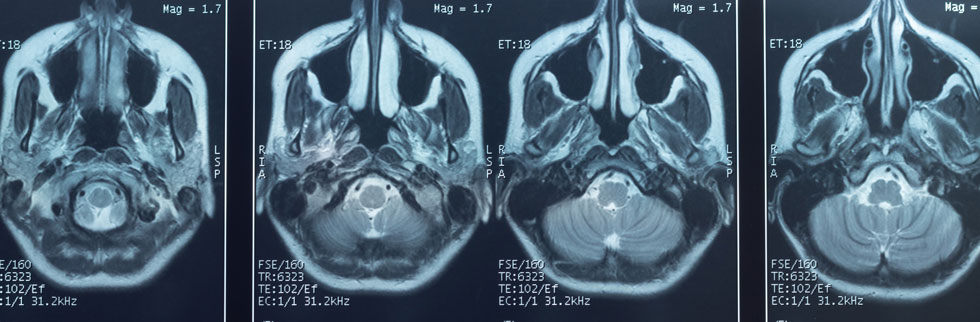
One of the most noteworthy articles to come out this past month was a Nature article comparing the brain structures of a large cohort of COVID-19 survivors before and after COVID-19. This study evaluated brain MRI scans of UK Biobank participants who were enrolled into a longitudinal multi-modal scanning study; participants were identified who had been scanned prior to having COVID-19, and re-imaged after receiving a diagnosis of COVID-19 (n=401). These participants were age, sex, and ethnically matched to uninfected controls who had had two scans with similarly elapsed time between the scans (n=384). The time interval between the two scans was an average of 3 years, and an average of 141 days from COVID-19 diagnosis in COVID-19 participants. The participants who had COVID-19 showed a greater decrease in gray matter thickness in the orbitofrontal cortex and parahippocampal gyrus when compared to controls, as well as greater decrease in overall brain volume with an additional 0.2 to 2% loss of gray matter or tissue injury between the two scans. They also displayed markers of tissue damage in areas connected to the primary olfactory cortex. Although these findings were mild to moderate overall, with some COVID-19 participants demonstrating no particular changes, these findings were statistically significant when compared to the control group. It is also worth noting that the vast majority of these COVID-19 participants were not hospitalized during their illness, with only 15 out of the 401 cases requiring hospitalization with COVID-19 (Douad 2022). There have been many reports of neurologic imaging findings in acute or post-acute COVID-19, including case reports and case series revealing such findings as white matter hyperintensities, microhemorrhages, hypoperfusion, and ischemic events in a variety of patterns, as well as rarer findings like hemorrhagic necrotizing encephalitis and ADEM (Ladopoulos 2021, Vogrig 2020, Paterson 2020). Olfactory bulb atrophy has also previously been reported, including in patients with pre-COVID imaging (Chiu 2020). There have also been a few cohort studies of neurologic imaging after COVID-19, including a PET study of 29 subacute COVID-19 patients who demonstrated FDG hypometabolism in the fronto-parietal regions (Hosp 2021). The recent Nature article by Douaud et al. is notable due to the large pre-COVID-19 imaging repository for this survivor cohort and control group, making the differences seen post-infection more likely to be related to COVID-19 (and less likely to be pre-existing).
Interesting longitudinal cognitive studies were published this past month, including a study out of Wuhan, China, which followed a large cohort of COVID-19 survivors who were age 60 years or greater, with a cohort of uninfected spouses as controls. Assessments (using the Informant Questionnaire on Cognitive Decline in the Elderly and the Telephone Interview of Cognitive Status-40) were taken at 6 months and one year after discharge from COVID-19-designated hospitals, with a total of 1438 COVID-19 survivors and 438 controls assessed at the final time point. Patients in the COVID-19 survivor group had lower cognition scores compared to controls at both 6 months and one year, with worse scores seen in patients who had severe COVID-19 compared to patients with non-severe COVID-19. The overall incidence of cognitive decline in the COVID-19 patient cohort was 12.45%, with higher risk for cognitive impairment at 12 months seen particularly in the patients with a history of severe COVID-19 (OR 9.10 in severe COVID-19 patients); interestingly, when the analysis compared close contacts to their paired COVID-19 patients, this increased risk of cognitive impairment was seen in both non-severe (OR 1.81) and severe COVID-19 (OR 5.91) patients (Liu 2022). Another study extracted real-world data from medical records to identify the proportion of new dementia diagnoses in patients who had had a diagnosis of COVID-19 pneumonia, and compared this to patients who were diagnosed with other types of pneumonia. They found an increased rate of new-onset dementia in patients diagnosed with COVID-19 pneumonia compared to controls with other types of pneumonia, particularly notable in patients greater than 7- years old (Qureshi 2022).
These studies raise concern for long term consequences of COVID-19 on the brain, but also raise many unanswered questions. Why are some people more susceptible than others? Do these patients have any underlying pre-symptomatic neurogenerative diseases? Is it possible that these changes may have occurred at the time of acute infection and now would be static, or might they progress or even improve? As time progresses, we will be able to understand the context of these studies better, particularly in light of COVID-19 protection through vaccination, as well as improved COVID-19 therapies. However, these studies bring to light that COVID-19 infection does indeed have varying effects on the central nervous system, and that we as neurologists should continue to be vigilant.
References
-
Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, Lange F, Andersson JLR, Griffanti L, Duff E, Jbabdi S, Taschler B, Keating P, Winkler AM, Collins R, Matthews PM, Allen N, Miller KL, Nichols TE, Smith SM. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022 Mar 7. https://doi.org/10.1038/s41586-022-04569-5 ⧉
-
Ladopoulos T, Zand R, Shahjouei S, Chang JJ, Motte J, Charles James J, Katsanos AH, Kerro A, Farahmand G, Vaghefi Far A, Rahimian N, Ebrahimzadeh SA, Abedi V, Papathanasiou M, Labedi A, Schneider R, Lukas C, Tsiodras S, Tsivgoulis G, Krogias C. COVID-19: Neuroimaging Features of a Pandemic. J Neuroimaging. 2021 Mar;31(2):228-243. Epub 2021 Jan 9. 10.1111/jon.12819 ⧉
-
Vogrig A, Gigli GL, Bnà C, Morassi M. Stroke in patients with COVID-19: Clinical and neuroimaging characteristics. Neurosci Lett. 2021 Jan 19;743:135564. Epub 2020 Dec 19. 10.1016/j.neulet.2020.135564 ⧉
-
Paterson RW, Brown RL, Benjamin L,et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020 Oct 1;143(10):3104-3120. 10.1093/brain/awaa240 ⧉
-
Chiu A, Fischbein N, Wintermark M, Zaharchuk G, Yun PT, Zeineh M. COVID-19-induced anosmia associated with olfactory bulb atrophy. Neuroradiology. 2021 Jan;63(1):147-148. Epub 2020 Sep 15. 10.1007/s00234-020-02554-1 ⧉
-
Hosp JA, Dressing A, Blazhenets G, Bormann T, Rau A, Schwabenland M, Thurow J, Wagner D, Waller C, Niesen WD, Frings L, Urbach H, Prinz M, Weiller C, Schroeter N, Meyer PT. Cognitive impairment and altered cerebral glucose metabolism in the subacute stage of COVID-19. Brain. 2021 May 7;144(4):1263-1276. doi: 10.1093/brain/awab009 ⧉
-
Liu Y, Chen Y, Wang Q, et al. One-Year Trajectory of Cognitive Changes in Older Survivors of COVID-19 in Wuhan, China: A Longitudinal Cohort Study. JAMA Neurol. Published online March 08, 2022. doi: 10.1001/jamaneurol.2022.0461 ⧉
-
Adnan I Qureshi, William I Baskett, Wei Huang, S Hasan Naqvi, Chi-Ren Shyu, New-Onset Dementia Among Survivors of Pneumonia Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection, Open Forum Infectious Diseases, Volume 9, Issue 4, April 2022, ofac115, https://doi.org/10.1093/ofid/ofac115 ⧉