Original article by Peter G.E. Kennedy M.D., PH.D., D.SC. published 29 October 2009 in World Neurology Vol 24 No. 5
Human African trypanosomiasis, which is also known as sleeping sickness, is a major killer disease in 36 countries in sub-Saharan Africa, where 60 million people are at risk for the disease and up to 50,000 people die annually from the infection.
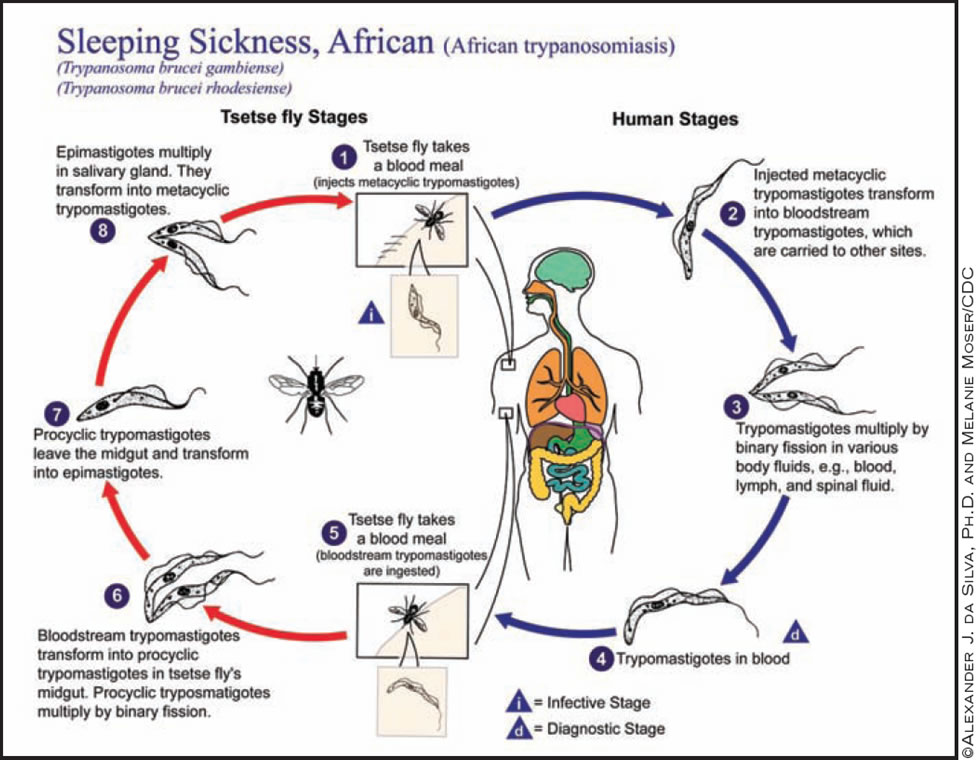
Human African trypanosomiasis (HAT) is caused by protozoan parasites of the genus Trypanosoma brucei, and is transmitted by the bite of the bloodsucking tsetse fly of the genus Glossina. Although HAT was almost brought under control mainly as a result of effective surveillance measures in the 1950s, there have been several resurgencies and epidemics since then, with a steady increase in the number of cases, largely due to disruption of social and surveillance infrastructure, especially during successive wars in affected regions. However, there is good evidence that the number of new cases is decreasing again because of improved patient surveillance.
Despite the fact that HAT is associated with a very significant morbidity and mortality, it is one of the world's "neglected diseases." Drug treatment for HAT is outdated and highly toxic, and this highly unsatisfactory situation reflects the chronic lack of financial investment from the developed world into new drug development for both stages of the disease. If untreated, or inadequately treated, the disease is invariably fatal.
There are two forms of the disease: East African HAT caused by Trypanosoma brucei rhodesiense (T.b. rhodesiense), and the West African variant caused by T.b. gambiense, which accounts for about 95% of cases of HAT. The disease caused by rhodesiense has a faster tempo than gambiense disease and leads to death if untreated in several weeks to a few months, whereas the course of gambiense disease may last many months to years.
Two Stages and a Range of Symptoms
There are two stages of HAT, the early (stage 1), or hemolymphatic stage, which occurs 1-3 weeks after the initial insect bite, and then the late (stage 2), or encephalitic stage, when the parasites cross the blood-brain barrier to enter the CNS (Ann. Neurol. 2008;64:116-26). In the early stage, the parasites spread in the bloodstream, lymph nodes, and systemic organs causing a variety of nonspecific symptoms, including malaise, headache, arthralgia, headache, and fatigue. Involvement of the heart, liver, spleen, skin, eyes, and endocrine system may also occur. Lymphadenopathy is typical of gambiense disease.
The range of symptoms and signs during the late stage is very wide. In most cases, there is a characteristic sleep disturbance with alteration of the normal sleep/wake cycle with a constant urge to sleep, and polysomnography demonstrates sleep structure abnormalities. There may also be motor disturbances, such as pyramidal weakness, extrapyramidal features, cerebellar ataxia, myelopathy, peripheral motor neuropathy, muscle fasciculation, and also frontal lobe features such as pout and palmarmental reflexes. Sensory disturbances can also occur, as may a variety of neuropsychiatric symptoms. Various types of visual involvement have also been described.
Untreated or unsuccessfully treated patients will rapidly deteriorate with seizures, cerebral edema, incontinence, and death. Typical autopsy findings in such patients will show a widespread meningoencephalitis, an extensive infiltration of cerebral white matter with inflammatory cells and pathognomic Mott cells, which are plasma cells containing immunoglobulin M eosinophilic inclusions.
Extensive data from both patients and a mouse model of the disease have implicated the key roles of pro- and counterinflammatory cytokines, astrocyte activation, and trypanosome-induced immune responses in causing the brain damage ( J. Clin. Invest. 2004;113:496-504).
No General Criteria to Aid Diagnosis
Sleeping sickness is diagnosed by identifying parasites in the peripheral blood or lymph node aspirates in the case of rhodesiense disease, and by serological means using the Card agglutination trypanosomiasis test (CATT) in the case of gambiense disease because in the latter case, there are usually few detectable parasites in the blood. There are no clinical suspicion criteria that can reliably distinguish the two disease stages, which may appear to merge into each other. All patients with proven HAT therefore require a lumbar puncture to examine the cerebrolspinal fluid (CSF) as that is the only current method of diagnosing CNS involvement.
Accurate staging of HAT is absolutely crucial because the drugs used for treating CNS disease are so toxic. If drug treatment is mistakenly withheld from a patient who has CNS disease then the patient will die, but giving highly toxic CNS drug therapy for early-stage disease carries the high risk of severe drug toxicity. This is one of the key dilemmas in managing patients with sleeping sickness. Unfortunately, there is no general consensus as to what criteria best define latestage disease, and this is one of the most problematic issues in HAT.
The WHO criteria for late-stage disease are the identification of trypanosomes in the CSF or a CSF white blood cell count (WBC) of greater that 5/mcL. But not everyone accepts this definition, and in West Africa a cutoff point of 20 CSF WBC/mcL is often used. Others have suggested a compromise figure of 10 WBC/mcL, but the actual presence of CSF trypanosomes is unequivocal proof that the CNS has been invaded. Although both CT and MRI scan abnormalities have been shown in the few patients who have been studied in Western hospitals, such facilities are not available in field conditions and are therefore primarily of value in investigating patients who have recently returned from Africa. There are about 50 cases a year of HAT diagnosed outside Africa, mainly in Western travellers returning from vacations to East African game reserves.
Toxic Drugs Hamper Treatment
Drug treatment of HAT is highly unsatisfactory and essentially relies on the use of four drugs, none of which can be given orally and which are so toxic that it is unlikely that they would have passed currently rigorous safety standards had they been introduced in recent years.
Early-stage rhodesiense disease is treated with intravenous suramin, and earlystage gambiense disease is treated with intramuscular pentamidine. For late-stage rhodesiense disease, the only effective drug at present is intravenous melarsoprol (Mel B), a highly toxic arsenical drug that was first used in 1949. It is given either as 2-4 courses of three times weekly injections or, more recently, as a 10-day course of injections. Although melarsoprol is generally effective treatment for late-stage HAT, in about 10% of patients, it is followed by a severe posttreatment reactive encephalopathy (PTRE), 50% of whom will die. Melarsoprol treatment has an overall fatality rate of 5%, which is remarkable.
The role of prophylactic corticosteroids in preventing the PTRE is controversial, although I personally would prescribe them. An alternative drug for late-stage gambiense disease is eflornithine (DFMO), which was first shown to be effective in 1981 but then became an "orphan drug." Because of efforts by Médecin Sans Frontières, working closely with the World Health Organization and the pharmaceutical industry, DFMO, which is expensive, was again made available for treatment of HAT. Eflornithine is less toxic than melarsoprol, but needs to be given intravenously over 14 days, which is not always practical in field hospitals. It is not without side effects and completely ineffective for treating rhodesiense infection. It has recently been suggested that a combination of eflornithine and nifurtimox is probably the optimum drug treatment for gambiense disease.
After effective treatment, all patients with HAT require regular follow-up, but this can be neither easy nor feasible. What are the prospects for better diagnosis and treatment of sleeping sickness? Despite many decades of underinvestment in HAT, there is now an increasing awareness of the importance and seriousness of the problem with increasing financial input from the developed world including from the Bill and Melinda Gates Foundation, WHO, the U.S. National Institutes of Health, and the Wellcome Trust.
Looking Toward an Ideal Solution
For better diagnosis, a rapid, user-friendly, inexpensive, reliable, and preferably noninvasive method of staging for both types of HAT is urgently needed. There are no new treatment drugs on the horizon and a promising oral drug for early- stage disease, DB 289, has been withdrawn near the end of a phase III clinical trial because of unexpected liver and renal toxicity. What is required, ideally, is a safe, inexpensive, oral drug that is effective for both early- and late-stage HAT. Such an advance would obviate the current dilemmas associated with CSF diagnosis of late-stage disease. ■

At time of print, Dr. Kennedy was the Burton Chair of Neurology and head of the Division of Clinical Neurosciences at the University of Glasgow, Scotland, and an honorary consultant neurologist at the Institute of Neurological Sciences, Southern General Hospital in Glasgow.