Switching from IVIG to FcRn inhibitors like efgartigimod in managing CIDP presents significant challenges, including the risk of early disease deterioration and mixed patient responses. Recent studies have highlighted severe relapses in some patients following the transition, underscoring the need for cautious and individualized treatment strategies. Additionally, unresolved issues with trial designs and safety monitoring emphasize the importance of refining clinical protocols to ensure both efficacy and patient safety during therapy transitions.
Navigating the switch from IVIG to FcRn inhibition in CIDP: Clinical insights
Authors: Chafic Karam
Editor's Choice
Journal of the Neurological Sciences. REVIEW ARTICLE| VOLUME 468, 123354, January 15, 2025
DOI: https://doi.org/10.1016/j.jns.2024.123354
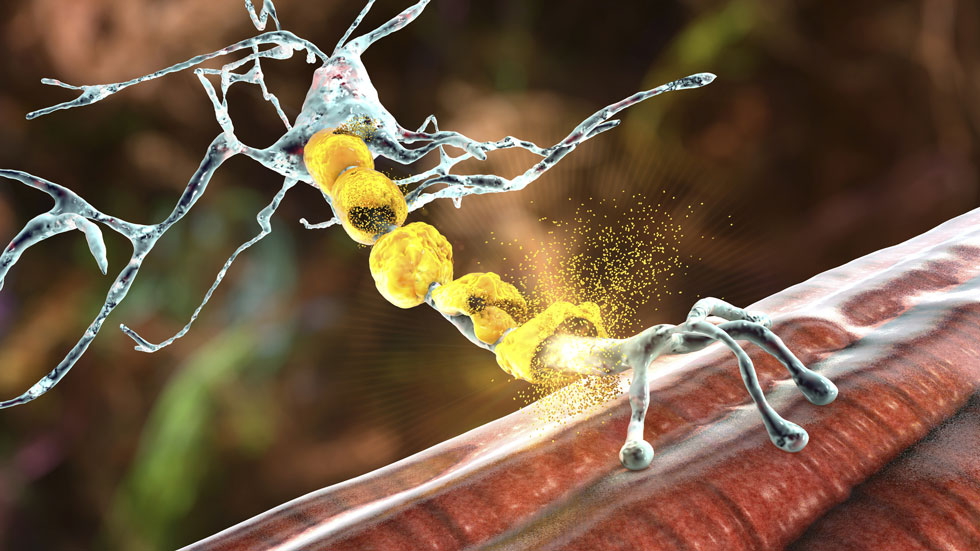
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a syndrome that comprises a heterogeneous group of rare, acquired, autoimmune, demyelinating polyneuropathies. The pathophysiology of CIDP, while not very well elucidated, involves both humoral (antibodies, complement) and cellular (autoreactive T cells) immune factors, with macrophage-induced demyelination. CIDP is a treatable condition, and patients can have full resolution of symptoms, especially when treated early and adequately. Unfortunately, the diagnosis can sometimes be difficult, especially in CIDP variants. We often see patients with delayed diagnosis or inadequate therapy resulting in irreversible axonal loss and residual disability.
Early deterioration of CIDP following transition from IVIG to FcRn inhibitor treatment
Authors: Todd Levine, Suraj Muley
Editor's Choice
Journal of the Neurological Sciences. REVIEW ARTICLE| VOLUME 468, 123313, January 15, 2025
DOI: https://doi.org/10.1016/j.jns.2024.123313
Highlights
- FCRn inhibitor therapy in CIDP patients on IVIg can lead to worsening of the disease.
- Safe approaches to switching CIDP patients on IVIg to FCRn inhibitor therapy may not be clear.
- Effectiveness of FCRn inhibitor therapy in IVIg treated CIDP patients is not clear.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an immune mediated demyelinating neuropathy that can lead to secondary axonal degeneration and irreversible weakness and disability. Early effective treatment is therefore necessary to minimize the degree of axonal degeneration. Prior to 2024 the only FDA approved therapy for CIDP was intravenous immunoglobulin (IVIg). In 2024, efgartigimod (Vyvgart-Hytrulo), a FCRn inhibiting therapy (FIT) was approved for treatment of CIDP based on the phase II Adhere study. In the controlled setting of the phase II clinical study patients who were stable on IVIg were taken off treatment to ensure that their disease was active, and patients who worsened were then treated with efgartigimod. The responders were then randomized (in phase B) to either placebo or continued efgartigimod treatment. In the real world setting it is not feasible to stop IVIg and let patients worsen before starting a FIT, thus the transition from IVIG to efgartigimod in a real world setting was not studied in the pivotal trial. We have treated nine patients with FIT in our practice and report findings of four of those patients who had severe relapse of CIDP after treatment. Five of the other patients neither improved nor declined with FIT. This raises questions about the issues related to transitioning patients from IVIG to efgartigimod.
Unresolved issues with efgartigimod in CIDP, and broader concerns for future trial design
Authors: Jonathan Katz, Liberty Jenkins, David Saperstein
Editor's Choice
Journal of the Neurological Sciences. REVIEW ARTICLE| VOLUME 468, 123355, January 15, 2025
DOI: https://doi.org/10.1016/j.jns.2024.123355
The U.S. Food and Drug Administration's (FDA) approval of efgartigimod, an FcRn antagonist, for the treatment of chronic inflammatory demyelinating polyneuropathy (CIDP) was based on the positive results of the ADHERE trial, which demonstrated that efgartigimod significantly outperformed placebo in a double-blind withdrawal study. However, a recent case series by Levine and Muley reports a concerning adverse outcome not highlighted in the trial. This new finding underscores the need for heightened safety vigilance and raises important questions about both the trial design and the broader implications for clinical research in CIDP.