
The expansion of telemedicine use in NMDs and development of clinically relevant but easy-to-use remote monitoring systems has potential to improve patient access to expert care.
 |
Remote clinical assessment enabled on a smartphone |
By M. S. Damian, MD, FEAN, FNCS, and Prof. P. Laforet, MD, PhD
Patients with neuromuscular disorders (NMDs) have diverse and complex care requirements, typically served by highly specialized centers. However, these may be geographically remote, and the COVID-19 pandemic underlined the system’s fragility by leading to widespread suspension of diagnostic, support, and rehabilitative services. Cancelled routine visits and limited outreach resulted in morbidity and even deaths. The demand for telehealth and remote care to help resolve this situation increased. This article describes the concept and current options using telemedicine in the care of people with NMDs.
Prior to COVID-19, telemedicine was mainly used to overcome geographical challenges in thinly populated or resource-poor regions, or for monitoring patients with impaired mobility at home. COVID-19 forced a hasty rethink of this position.
Overall, the use of telemedicine in NMDs increased during the COVID-19 pandemic, but telemonitoring was used considerably less.
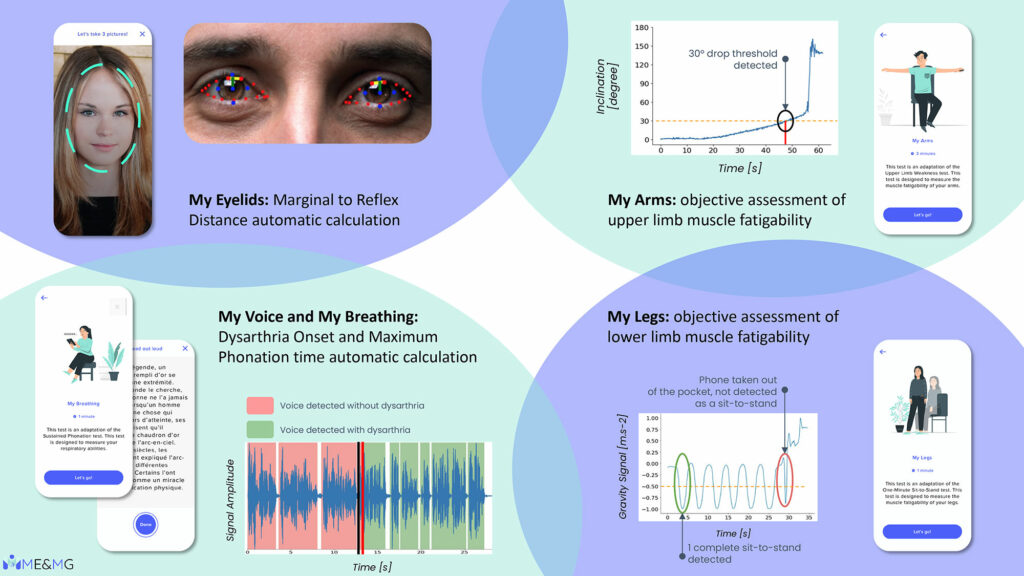
Telemonitoring found its first application in clinical trials to optimize remote clinical assessment, but also to improve trial recruitment and monitoring. Reliability and strong correlations between wearable physical activity monitors (sensor-based systems using activity watches or body-worn sensors, PAMs) and neuromuscular measures confirmed PAMs’ utility as outcome measures and in long term monitoring. Mobility data can be gathered by PAMs, or by ambient measurement systems (AMS), which passively measures movement such as ambulation speed, rise-to-stand speed, and arm-raise speed when someone is in range of a sensor.
Remote monitoring of life-supporting technology, such as home mechanical ventilation (HMV), requires regular monitoring of physiological variables (spO2, spCO2, respiratory rate) by carers supported by specialist outreach, and requires a continuous data link to the monitoring center for analysis and troubleshooting. It can enable remote initiation of HMV and may reduce costs, and may help predict exacerbations, allow remote interventions and adjustments. Challenges about data security and privacy, caregiver involvement and acceptance, availability of high-speed internet, and misconceptions around time needed, remain.
The expansion of telemedicine use in NMDs and development of clinically relevant but easy-to-use remote monitoring systems has potential to improve patient access to expert care, even in situations where direct face-to-face access is interrupted, as in the recent pandemic, or where scarce resources or geography prevents patient access to specialist care. Going forward, telemedicine might expand the availability of high-quality specialist care to patients in low-income societies, who hitherto have had little access. Recent developments in effective treatment can also be seen as an obligation on global medicine to explore how inequality in provision can be mitigated — telemedicine technology may advance us one step in this direction. •
M. S. Damian, MD, FEAN, FNCS, works at the Essex Cardiothoracic Centre, in Basildon, UK, and Prof. P. Laforet, MD, PhD, works in the Neurology Department, Raymond Poincaré Hospital, APHP, Garches, APHP, FHU PHENIX, Centre de référence des maladies neuromusculaires Nord Est Ile-de-France in Filnemus.
Editor's Choice
World Neurology | Mar-Apr 2024, Volume 39, No. 2








